A) INTRODUCTION
1) Thermal Tests- Cold Test, Heat Test
2) Electric Pulp Test
3) Anesthetic Test
4) Test Cavity
1) Thermal Tests
a) Heat Test
Materials used
Electrical heat carrier
Hot gutta-percha stick (>65.5° C)
Others
–– Hot water under rubber dam isolation
–– Hot burnisher
–– Hot compound
–– Dry rubber polishing wheel
Electrical Heat Carrier
If there is no response, the hot substance can be moved to the central portion of the crown or closer to the tooth cervical margin.
When a response occurs, heat should be removed immediately.
Care should be taken to avoid using excessive heat or prolonged application of heat to the tooth
Hot Burnisher
How to do a cold test for teeth?
b) Cold Tests
Material Used
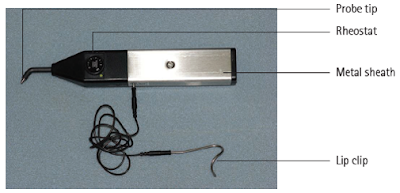
How to use a pulp tester?
2) Electric Pulp Test
The accurate diagnosis of the true
histological status of the pulp is of significant importance for treatment
planning.
What is Pulp sensibility test?
What is Pulp sensibility test?
Pulp Sensibility Testing- Assess the Neural sensitivity of the pulp
What is Pulp Vascularity Test?
What is Pulp Vascularity Test?
Pulp Vitality Testing- Assess the
vascularity of the pulp
What is Pulp Sensivity ?
What is Pulp Sensivity ?
Pulp Sensitivity- Condition of the Pulp Being Very Responsive to
a Stimulus.
B) NEURAL SENSIBILITY TESTS
2) Electric Pulp Test
3) Anesthetic Test
4) Test Cavity
1) Thermal Tests
a) Heat Test
Materials used
Electrical heat carrier
Hot gutta-percha stick (>65.5° C)
Others
–– Hot water under rubber dam isolation
–– Hot burnisher
–– Hot compound
–– Dry rubber polishing wheel
Electrical Heat Carrier
Heat carrier instrument that
can deliver a controlled temperature to the tooth is preferable
Hot Gutta Percha Sticks
The heat is applied to the occlusobuccal third of the exposed crown.
If there is no response, the hot substance can be moved to the central portion of the crown or closer to the tooth cervical margin.
When a response occurs, heat should be removed immediately.
Care should be taken to avoid using excessive heat or prolonged application of heat to the tooth
Hot Burnisher
Held about 1–2 mm away from the
labial or buccal surface of the tooth. Avoid touching the
tooth surface as the hot instrument will burn the enamel and
leave a black spot.
Other Tests
A different technique is required for the application of hot water. The tooth to be tested is isolated under a rubber dam. The tooth is then immersed in “coffee-hot” water delivered from a syringe, and the patient’s reaction is noted.
Other Tests
A different technique is required for the application of hot water. The tooth to be tested is isolated under a rubber dam. The tooth is then immersed in “coffee-hot” water delivered from a syringe, and the patient’s reaction is noted.
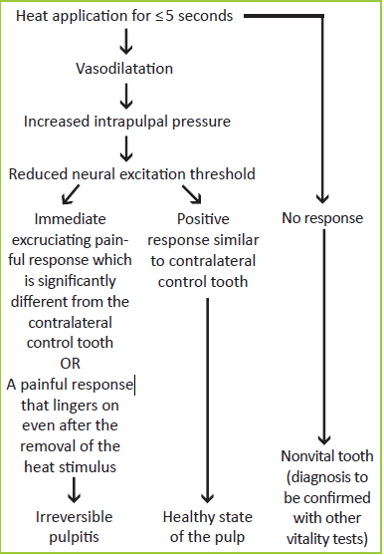
Mechanism of Action
How to do a cold test for teeth?
b) Cold Tests
Material Used
Endo ice → 1,1,1,2 tetrafluoroethane
(-26 C)
Mixture of gases
(propane/butane/isobutene)(-50 C)
CO2 snow (Dry ice) (-78 C)
Pencil of
ice
Ice cold water under rubber dam
isolation
Ethyl chloride- (-4 C)
Dichlorodifluoromethane- (-21 C)
Endo ice → 1,1,1,2 tetrafluoroethane (-26 C)
The most common method is to apply a cotton pellet saturated with 1,1,1,2 tetra-fluoroethane to the tooth being tested.
it has a temperature of about −26°C
when first
sprayed from the pressurized can but this reduces to about
−18.5°C in the mouth.
Another simpler method of applying cold to a tooth is by following these steps: wrap a sliver of ice in wet gauze, place it against the facial surface of the tooth, and compare the reaction to a control tooth.
Pencils of ice can be made by filling discarded anesthetic carpules with water and freezing them in an upright position in a refrigerator
Dachi and associates recommended that a quarter- inch-diameter cone of ice be placed against a tooth for 5 seconds to quantify cold testing.
CO2 snow (Dry ice) (-78 C) (Odontotest-Dry ice)
Carbon dioxide (dry ice) snow has also been used for application of cold to teeth.
The use of dry ice has been described by Ehrmann.
Because the temperature of dry ice is –78°C, one is able to penetrate full-coverage restorations and elicit a reaction from the underlying tooth to the cold.
Mixture of gases (propane/butane/isobutene)(-50 C)
The propane/butane/ isobutane mixture
temperature is approximately −50°C and reduces to
about −28°C in the mouth.
Mechanism
How to use a pulp tester?
2) Electric Pulp Test
The
objective is to stimulate a
pulpal response by subjecting the tooth to an increasing
degree of electric current.
The electrode is placed against the incisal third enamel surface of the isolated and
dried tooth crown using toothpaste as an electrolyte
The electrode is
placed against the mid-third of the mesiobuccal cusp of molars and buccal cusp
of premolars
Normal
response: A positive response is a response that
occurs at the same neural excitation threshold as
the control tooth
Negative
response: This denotes a nonvital tooth, which fails to respond even when the tester is set to the highest electrical excitation value.
Early
response: This
denotes a
diseased state of pulp as the tooth responds to a threshold which is less than that
of the control
tooth
Delayed
response: This also denotes a diseased
state of
the pulp wherein the tooth responds at a
significantly higher electrical excitation level than compared to
the control tooth
False
Positive Response-
1)Partial
Pulp Necrosis
2)High
Anxiety
3)Ineffective
tooth isolation
4)Contact
with metal restoration
False
Negative Response-
1)Calcified
Canals
2)Recently
Traumatized tooth
3)Immature
apex
4)Drugs
that increase pain threshold
5)Poor
contact of pulp tester
The diagnostic accuracy of cold test is 86%, the electric pulp test is 81%, and heat test is
71%. Hence, clinically, a combination of cold test followed by EPT is recommended.
Cold test
is the most effective sensitivity test for immature permanent
teeth
3) Anesthetic Test
The
objective is to anesthetize one tooth at a time until the pain disappears and is
localized to a
specific tooth
Using
either
infiltration
or the
intraligament injection, inject the most posterior tooth
in the area suspected of being the cause of
pain.
The
anesthetic test is obviously a last resort test and has an
advantage over the “test cavity,” during which iatrogenic damage
is possible
4) Test Cavity
It is
performed when other methods of diagnosis have failed. The test cavity is made by
drilling through
the enamel–dentin junction of an unanesthetized tooth.
The drilling
should be done
at high
speed and with a water coolant. Sensitivity or pain
felt by the patient is an indication of pulp vitality
C) PULP VASCULARITY TESTS
True
vitality status can be ascertained only
when we are able to assess the vascular or blood supply to the tooth
(1) Laser
Doppler Flowmetry
(2)
Pulse oximetry
(3)
Others
(i)Dual-wavelength
spectrophotometry
(ii)Crown
surface
temperature
(iii)Transillumination
with Fiberoptic Light
(iv)Plethysmography
(v)Radiation
Probe Using Xenon Radioisotope
1) Laser Doppler Flowmetry
Noninvasive
method of
assessing and accurately measuring the rate of
blood flow in a tissue
Developed by Tenland in 1982 and
later by
Holloway in
1983
Uses
a laser source that is aimed at the pulp, and the laser light travels to the
pulp using the dentinal tubules as guides.
This
principle is used to ascertain the presence of blood movement
within the pulp space
The
laser light is transmitted through a
fiberoptic source and placed on to the tooth surface.
The
light enters the tooth and gets absorbed by
the red blood cells which lead to a shift in the frequency
of the scattered light.
This occurs due to
the Doppler principle.
This shift in frequency does
not occur in light that is absorbed by stationary objects.
The proportion of Doppler shifted light is detected with the help of a photodetector
it
is potentially used to differentiate a healthy, traumatized tooth
with reduced blood supply from a nonvital tooth
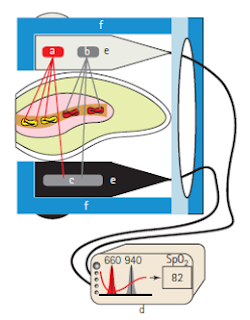
2) Pulse Oximetry Test
Noninvasive
method
to measure
the oxygen
saturation levels with the help of a finger, ear, or foot probes
Two light-emitting
diodes
Red
light (660
nm)
Infrared
light (940
nm)
Photodetector
on
the opposite
side of
the vascular bed
Oxygenated
hemoglobin and deoxygenated hemoglobin absorb different amounts of red and
infrared light
The pulsatile
change in the blood volume causes periodic changes in the amount of
red and
infrared light
absorbed by the vascular bed before reaching the
photodetector.
Pulsatile
change in red and infrared light detected by photodetector
3) Dual Wavelength Spectrophotometry
Uses visible light that is filtered
and guided to the tooth by fibreoptics.
Thus unlike Laser light, added eye
protection is unnecessary for the patient and
the operator.
Noninvasive and yields objective
results.
4) Measurement of Surface Temperature of Tooth
Pulp becomes nonvital, the
tooth no longer has internal blood supply, thus
should exhibit a lower surface temperature
than that of its
vital counterparts.
Fanibund in 1985 showed that it is
possible to differentiate
by means of crown surface temperature,
distinct difference between vital and nonvital teeth.
5) Transillumination with Fiberoptic Light
It is a system of illumination
whereby light is passed through
a finely drawn glass or plastic
fibers by a process known as
total internal reflection.
By this method, a pulpless tooth that is not noticeably discolored may
show a gross difference in translucency
when a shadow produced on a mirror is
compared to that of
adjacent vital teeth
6) Plethysmography
Assessing the changes in volume and
has been applied to the investigation of
arterial disease because
the volume of the limb or organ
exhibits transient changes
over the cardiac cycle.
The same principle can be used to assess tooth vitality.
Presence or absence of a
wave form can indicate the status of the
tooth.
7) Radiation Probe Using Xenon Radioisotope
The tooth to be tested injected with xenon in saline.
A lead shield placed over the tooth and radiation counts
taken every 10 seconds for 15 minutes, using a small cadmium telluride
radiation probe.
Radiation counts detected from both
vital and pulpless teeth
Pulpless teeth report relatively
constant counts for the duration of the experiment (200-300).
In vital teeth the initial counts
were much higher (718-981).