Dentin
Dentin is a hard tissue, which is
also mildly elastic in nature.
Also called substantia eburnea
Forms the
bulk and provides general form and shape to the tooth
Covered by the enamel in the crown
and by the cementum in root
Determines the
shape of the crown and also the number and size of the roots
COLOR- Pale yellow,
contributes to the colour of the crown of the tooth
HARDNESS- Dentin is harder than bone and cementum
but softer
than enamel
VISCOELASTIC- Even though dentin is rigid, it is
elastic in
nature,
which permits slight deformation.
STRENGTH- Higher compressive and less tensile
strength than enamel
PERMEABLE- The tubular structure of dentin
makes it permeable
RADIOLUCENT- Dentin is more radiolucent than
enamel because of its reduced mineral content
SENSITIVITY- Dentin differs from enamel in that
it is
sensitive and forms throughout life at the expense of the
pulp
The modulus of elasticity-1.67
x 106 PSI.
Density 22.1 gm/mm
KHN 68
Chemical Properties
Dentin
is made up of approximately 70% inorganic material,
20% organic material and 10% water by weight
50%
inorganic material, 30% organic material and 20% water by volume
The
inorganic portion
is in the form of calcium hydroxyapatite crystals
crystals
are similar in shape to
those of enamel, they are smaller in size, rich in carbonate
and poor in calcium when compared with those in enamel
The
collagen fibres, constituting 90%
of the organic matrix, are mainly made up of type
I collagen and and ground substance
of mucopolysaccharides, glycosaminoglycans, proteoglycans,
and phosphoproteins with small amounts of citrate, chondroitin sulfate, insoluble protein and
lipid.
- Read About
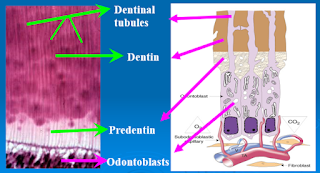
Structure of Dentin
The
dentinal tubules are sigmoid (‘S’) shaped curved Structures
which run perpendicularly from the pulp toward the periphery
Near
the root tip, incisal edges and cusps, the dentinal tubules are almost straight
The
first convexity of the doubly curved dentinal tubules is directed towards the apex of the
tooth
They are perpendicular to
dentinoenamel junction and cementoenamel junction
Two
bends making up the S-shape are called the primary curvatures
Secondary
curves- During the deposition of dentin, the odontoblast makes
slight undulations that creates wavy dentinal tubules. Waviness
of the dentinal tubules is called secondary curves.
The
diameter of
the dentinal tubules is larger at the pulpal side (1.5 to 3 microns) than at the dentino-enamel junction
(one-micron)
The
number of tubules per unit area at the pulpal end is nearly four to five times
more than at the outer surface of the dentin
The
ratio between the outer and the inner surfaces of dentin on an average is 5:1
Therefore, the tubules are farther apart in the outer layers and
closer together near the pulp
Number- Pulpal : outer surfaces of the dentin- 4:1
Number
per sq. mm – 50,000- 90,000
The root dentin has lesser tubules compared to the crown
The
dentinal tubules show more branching at their terminal parts
The
lateral branches are called as canaliculi or microtubules
These
microtubules originate at right angles to the main tubules every one to two
microns along its length
The
dentinal tubules contain the odontoblastic processes
and a thin organic sheath lining the dentinal tubules. This layer is called lamina limitans
A few dentinal tubules may
extend through the DEJ into enamel for several millimeters called enamel
spindles
CLINICAL IMPLICATIONS OF DENTINAL TUBULES
Make the dentin permeable, providing a
pathway for the invasion of caries
Microscopic examination of infected
dentin shows that the dentinal tubules are packed with microorganisms well ahead
Drugs and chemicals present in a variety of dental restorative materials can also diffuse through the dentin and create pulpal injury
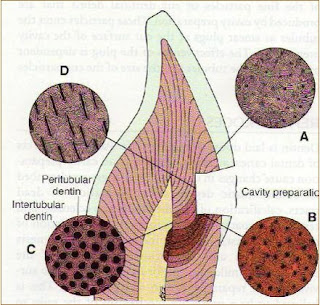
B) PERITUBULAR OR INTRATUBULAR DENTIN
Dentin that immediately surrounds
the dentinal tubules and is termed peritubular dentin or intratubular dentin
More highly mineralized (9%) &
lacks collagen fibres than inter-tubular
dentin
The intratubular dentin is
formed after
the intertubular dentin formation occurs
Approximately two times
as thick
in outer dentin than in inner dentin
C) INTERTUBULAR DENTIN
Main Body of Dentin- Present between
the dentinal tubules or peritubular dentin
Located between the Peritubular
Dentin
About one half of its
volume is
organic matrix, mainly collagen fibrils.
Highly mineralized- Retained after
decalcification
Innermost Dentin- Non Mineralized
Located Adjacent to Pulp
First formed Dentin
Width 2-6 micron
About one half of its
volume is
organic matrix, mainly collagen fibrils.
As collagen fibres undergo mineralization
at pre-dentin – dentin junction ,predentin becomes dentin and a new layer of
predentin forms circumpulpally
E) ODONTOBLASTIC PROCESSES
Cytoplasmic Extension which extend into
the dentinal tubules
The cells are present in the
peripheral pulp
at the pulp- predentin border
Diameter of
3–4 μm when it enters the dentinal tubule tapers to
about 1 μm as it extends further into the tubule.
Cell bodies of the odontoblast are about
7 microns in diameter and about 40 microns in length.
Therefore, the odontoblastic processes
become narrow to
about half
the size of the cell as they enter the dentinal tubules.
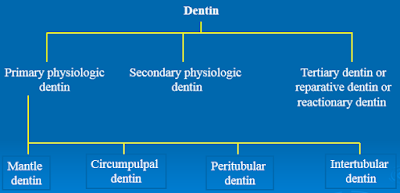
F) TYPES OF DENTIN
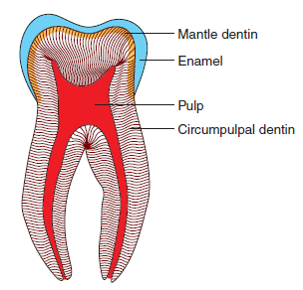
G) PRIMARY DENTIN
Primary
dentin is formed prior to the complete eruption of
the teeth and root completion
It forms the major bulk of the
dentin
It is composed of mantle dentin and circumpulpal
dentin
Primary dentin fulfills the initial formative function of the pulp
First formed dentin close to DEJ
20 micron thick below the DEJ
Type III collagen fiber
(Vankorff’s fibres)
Fibers are larger, loosely packed
& perpendicular to DEJ
Less Mineralized
Shows fewer defects than circumpulpal
dentin
Circumpulpal Dentin
Formed dentin close to Pulp
Bulk of tooth
Collagen fiber
Diameter
0.05 micron
Fibers are smaller, closely packed
More Mineralized
H) SECONDARY DENTIN
Formed after root completion and
eruption
Regular, Narrow band around the
pulp
Few dentinal tubules than primary
Bend of tubule at junction of
primary and secondary dentin
Grows slowly and reduce the size of
pulp cavity
Grows on floor and wall of pulp
cavity
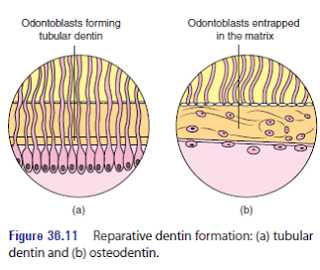
I) Tertiary Dentin/reactive
/ reparative / irregular Secondary
dentin
Formed in
response to
various stimuli
such as attrition, caries or restorative dental procedure.
Protect
the
pulp from the inward spread of noxious materials along the dentinal tubules
(like bacterial toxins etc.)
Reactionary or Regenerated Dentin
1) If
odontoblasts
are survived after exposure to the operative procedures,
abrasion, erosion or caries and produce dentin then
this dentin is known as reactionary or regenerated dentin.
2)
Irregular appearance with fewer tubules
Reparative Dentin
1)
Formed by
the newly differentiated
odontoblast-like cells that replace the original odontoblasts that
have been destroyed by insult/stimulus.
Newly differentiated odontoblast-like cells
may get entrapped
in the
matrix they form to produce osteodentin
External
stimuli
such as slowly progressing caries, attrition or
erosion.
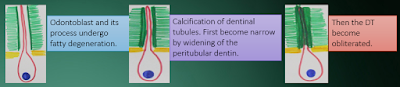
Fatty
degeneration of Odontoblasts and its process
Laying
down
of apatite
crystals later
forms a fine meshwork
Obliterating
the lumen
of the tubule completely
Tubule
is
completely filled with mineral
The refractive
indices are equalized and becomes transparent
it appears
light in
transmitted light and dark in reflected light.
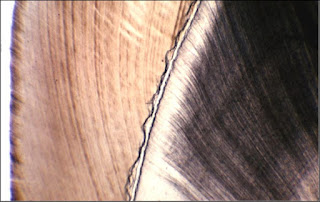
K) DEAD TRACTS
Odontoblastic
cell
processes in the dentinal tubules are degenerated, leaving behind empty,
air-filled tubules referred to as “dead tracts”.
Appear
black in transmitted light and white in reflected light.
Demonstrate
decreased sensitivity.
Probably
the initial step in formation of sclerotic dentin.
More often
seen in the region of narrow pulp horns in coronal dentin
More commonly
in older teeth and demonstrate reduced sensitivity
Calcification
of dentin in some areas occurs in a form of globular pattern.
These globules fuses together to
form homogenous substance
Sometimes globules in some areas failed
to fuse. Area of organic matrix between the globules remain uncalcified or
partially mineralized. These areas bonded by the curved outlines of the
adjacent globules.
Striations
in dentin
Perpendicular
to dentinal tubules
Reflects the daily rhythmic
recurrent deposition of dentinal matrix
Indicates- Growth pattern of dentin
Some incremental lines are accentuated because of
disturbance in matrix and mineralization process, such lines are called contour
lines of OWEN
Hypocalcified
area seen in
those teeth, where dentin is partly formed before
birth and partly formed after birth.
All deciduous
teeth and first permanent molars.
Represent
the
disturbance in mineralization due to the abrupt change in environment
Adjacent
to Cementum. increases in amount from the cementoenamel junction
to the apex of the root
The
granular layer represents the looped terminal portion of the
dentinal tubules in the root dentin
similar
to the
branching and
beveling of the dentinal tubules at the dentinoenamel junction
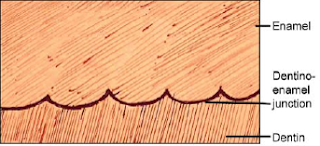
The
junction between the enamel and dentin is irregular and is
described as scalloped. The convexities face the dentin whereas the concavities face enamel.
R) PREDENTIN PULP JUNCTION
Made
up of dense collagenous fibers and is present between the
uncalcified dentin (predentin) and pulp.
S) DENTIN PREDENTIN JUNCTION
Dentin
predentin junction is the interface between the calcified and
uncalcified newly formed dentin called predentin
T) DENTINO-CEMENTUM JUNCTION
There
is a smooth line junction between the dentin and cementum in
permanent teeth.
The
cementodentinal junction in deciduous teeth, however, is sometimes slightly
scalloped. The
attachment of cementum to dentin is quite firm.
Dentinal Sensitivity
Exposed
dentin is very sensitive. Three main theories have been
proposed to explain dentin sensitivity
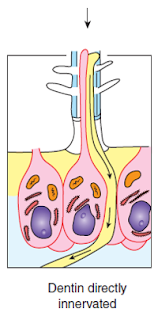
A) Direct Neural Stimulation Theory
B) Transduction Theory
C) Hydrodynamic or Fluid Theory
This
theory states that the nerve endings inside the dentinal tubules
are directly stimulated and cause sensitivity/pain.
Drawbacks
Even
though nerve endings are seen inside the dentinal tubule,
they are confined to the inner dentin and are absent in the outer dentin
Topical
application of the local anaesthetic to the surface
of dentin does not eliminate dentin sensitivity.
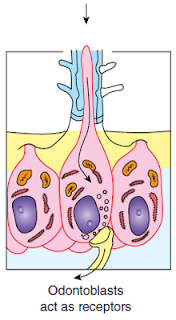
This
theory states that various stimuli stimulate the odontoblastic process
which conducts the impulses to the nerve endings located in the inner dentin
Drawbacks
Neurotransmitter
vesicles are absent in the odontoblastic process
There
is no synaptic relationship between the odontoblastic process
and the nerve endings.
Dentin
sensitivity
is due to the
movement of
fluid inside the dentinal tubules
Stimuli
such
as heat, osmotic pressure and drying can cause outward
movement of fluid
Cold
stimulus causes inward movement of fluid
Causes
mechanical
disturbance of the
nerve endings
which are present in the inner dentin and are close to the odontoblasts and their
process
The
free nerve endings in the plexus of Raschkow sense these disturbances, resulting in
sensitivity/pain
This
widely accepted theory proposes that nerve endings act as mechanoreceptors
Tags:
Dental Histology



What do you think about casino, slots, slot machines?
ReplyDeleteCasinos are mostly played 파주 출장마사지 for fun, especially slot machines. 군포 출장안마 These machines are 영주 출장마사지 the same kind of machines that 목포 출장샵 can be used in casinos all 목포 출장안마 around the world.