The term Monoblock was introduced by Dr. Pierre Robin in 1902 in the field of Orthodontics which refers to a “Single unit”.
Franklin R.Tay first described the concept of monoblock in endodontics.
The monoblock in root canal is used to signify a scenario where in the canal space is perfectly filled with a gap-free, solid mass that consists of different materials and interfaces with the purported advantages of simultaneously improving the seal and fracture resistance of the filled canals.
Success of root canal therapy depends upon thorough cleaning, shaping and three dimensional obturation. In order to obtain a hermetic seal, the core filling materials and the sealers used to seal the root canal must create different interfaces forming a monoblock.
With the rigidity of the root weakened by endodontic and restorative instrumentation, the sealing quality and tooth strengthening potential of endodontic replacement monoblocks become important issues. Strengthening of immature root canals with open apices and reduced circumferential dentin thickness are also issues of concern.
Based upon the interfaces monoblocks are classified in to
Primary monoblock
Secondary monoblock
Tertiary monoblock.
A primary monoblock has only one interface that extends circumferentially between the material and the root canal wall.
Examples-
Hydron
MTA
Polyethylene fibre post-core systems
Biogutta
iRoot SP (EndoSequence BC Sealer)
Hydrone
Introduction
In the late 1970s, a Poly HEMA containing root filling material (Hydron; Hydron Technologies) was marketed for en mass filling of roots. The material garnered significant interest as a potential successor for sealer-dependent lateral and vertical gutta-percha (GP) obturation.
Advantage
Its purported qualities included ease of use, nonirritating nature, adaptability to walls, and ability to calcify in the event of extrusion.
Disadvantage
However this material became obsolete in the 1980s in view of discrepancies between the manufacturer’s claims and laboratory/clinical findings.
Hydron-filled root canals exhibited extensive leakages and Residual moisture within root canals notably hampered polymerization to form soft hydrogels that were extremely permeable and leachable.
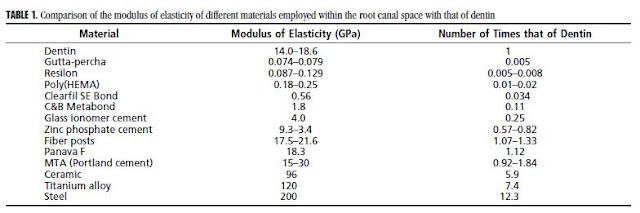
Modulus of elasticity of Hydron ranges from 180 to 250 MPa. On the contrary in order to reinforce roots, the modulus of elasticity of a root filling material would need to approximate that of dentin (i.e., 14,000 MPa).
MTA
Introduction
MTA is a Calcium silicate based material that has been made available since 1998
Used as an apexification material represents a contemporary version of the primary monoblock in attempts to strengthen immature tooth roots
MTA is composed principally of Portland cement with the addition of bismuth trioxide to render it radiopaque
Advantage
It is prudent to point out that the so-called high push out bond strength (ca. 38–40 MPa).
Interaction of the released calcium and hydroxyl ions of MTA with a phosphate-containing synthetic body fluid results in the formation of apatite-like interfacial deposits. The formation of these nonbonding, gap-filling apatite deposits probably also accounts for the seal of MTA in orthograde obturation and perforation repair.
The compressive elastic modulus of Portland cement increases after 14 days to 15 GPa (i.e., 15,000 MPa). Unlike Hydron, MTA should theoretically be able to strengthen roots.
Ability to stimulate cementogenesis in apexification and root end fillings
Disadvantage
Being an entirely inorganic material, Portland cement undergoes chemical shrinkage after hydration. Thus, a certain amount of volumetric shrinkage should also occur during the setting of MTA.
MTA is not bonded to dentin. The inability of MTA to strengthen roots is probably a combination of its lack of bonding to dentin and its low strength in tension, although it has high stiffness in compression
Polyethylene fibre post-core systems
A fiber composite laminate endodontic post and core system based on a woven polyester bondable ribbon had been introduced. This reinforcement material is composed of plasma treated ultra-high molecular weight polyethylene fibers woven into three dimensional structure, leno wave or triaxial braid.
Polyethylene fibre post-core system such as Ribbond (Ribbond Inc., Seattle, WA, USA) can create a primary monoblock in a root canal.
Impregnation of polyethylene fibre with a dual curable adhesive system (Belli & Eskitascioglu 2008).
Impregnated fibre is then condensed into the root canal in combination with a dual curable resin cement
Moreover fibres adapt well to root canal hence significant canal enlargement is not necessary. bonding agent to build-up endodontic posts and cores.
MOE similar to dentin.
A study by Singh et al reported that cyclic loading reduced the retention of all posts but was lesser for the polyethylene posts compared to glass fibre posts.
Similarly data on leakage studies indicate resin-supported polyethylene fiber dowels and glass fiber dowels tested exhibited less microleakage compared to zirconia dowel systems.
it provides good fracture resistance with increased incidence of repairable fractures in structurally compromised canals
However, a study by Jindal et al reported that endodontically treated teeth restored with
glass fiber posts showed increased fracture strength and favorable mode of fracture as compared to poloethylene fibre posts.
Biogutta
A recent addition to the category of primary monoblock in denstistry is the Biogutta. This product contains bioactive glass of the 45S5 [The 45S5 name signifies glass with 45 wt. % of SiO2 and 5:1 molar ratio of Calcium to Phosphorus] type incorporated into polyisoprene, the matrix polymer of gutta-percha.
Bio GP Points composed of bioceramic materials creates monoblock obturation in canal wall with bioceramic-based sealer.
Manufacturers claim the material is self-adhesive with immediate sealing of the canal system.
This has been attributed to the formation of Calcium Phosphate crystals on the material’s surface in a wet environment.
Preliminary studies report good push out bond strength to the canal dentin when compared with conventional gutta percha.
iRoot SP
Injectable Root Canal Sealer (Innovative BioCeramix Inc., Vancouver, BC, Canada), is an example of a calcium phosphate silicate-based cement.
Ability to form hydroxyappetite during the setting process and ultimately create a chemical bond between dentinal wall and the sealer.
These are convenient, premixed, ready-to-use, injectable white cement paste developed for permanent root canal filling and sealing applications.
These materials consists of two circumferential interfaces, one between cement/Sealer and dentin and other between the cement/Sealer and core material.
Examples
Resilon based systems
Fibre re-inforced posts.
iRoot SP with Gutta-Percha
By definition, conventional root canal obturations may be regarded as secondary monoblock systems on account of the two interfaces (one between sealer and dentin, second between sealer and conventional guttapercha condensed into a homogenous mass).
However the lack of sealer bond to dentin or guttapercha and the trivial values of modulus of elasticity (80 MPa) that are 175–230 times lower than dentin are contrary to the fundamental concepts of the ‘monobloc effect’.
Resilon
Resilon (2004) is a thermoplastic, synthetic, polymer-based obturation material
it is the first true bondable root canal filling material.
it is composed of dimethacrylate resin, bioactive glass as a filler, bismuth oxychloride, radiopaque barium sulfate, and polycaprolactone
The system consists of three parts:
1. Resilon – a thermoplastic synthetic polymer-based (polyester) root canal filling material, as the major component;
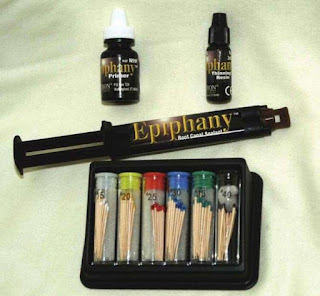
2. Epiphany sealer – a dual-cure methacrylate resin-based composite
3. Self-etching primer - which prepares the canal wall to get in contact with Resilon and the sealer.
Resilon core closely adapting to the EpiphanyTM sealer and in turn the EpiphanyTM sealer adhering to the dentin walls via “resin tags”(mono-block)
The possibility that Resilon filled canals would be more able to withstand bacterial penetration as a result of this “Resin Monoblock System (RMS)”
Available in standardized points in various tapers, accessory points and pellets for use with Obtura II delivery system.
Various techniques can be employed to place this material in the canal-
• Single-cone Method
• Cold Lateral Condensation
• Thermoplastic Techniques
Resilon is the only bondable root filling material that may be used for either lateral or warm vertical compaction techniques.
Disadvantage
Marketed as a monoblock system by using conventional gutta-percha cones that are surface coated with glass-ionomer fillers.
Franklin R.Tay first described the concept of monoblock in endodontics.
The monoblock in root canal is used to signify a scenario where in the canal space is perfectly filled with a gap-free, solid mass that consists of different materials and interfaces with the purported advantages of simultaneously improving the seal and fracture resistance of the filled canals.
Success of root canal therapy depends upon thorough cleaning, shaping and three dimensional obturation. In order to obtain a hermetic seal, the core filling materials and the sealers used to seal the root canal must create different interfaces forming a monoblock.
With the rigidity of the root weakened by endodontic and restorative instrumentation, the sealing quality and tooth strengthening potential of endodontic replacement monoblocks become important issues. Strengthening of immature root canals with open apices and reduced circumferential dentin thickness are also issues of concern.
Prerequisites for Monoblock
1.The materials that constitute a monoblock should have the ability to bond strongly and mutually to one another.
2. These materials should have a modulus of elasticity that is similar to that of the substrate (i.e Dentin- 14-18.6 GPa or 14000 MPa)
Sealability
Successful root canal treatment banks on the achievement and maintenance of a hermetic seal chemically and or micromechanically, along canal system.
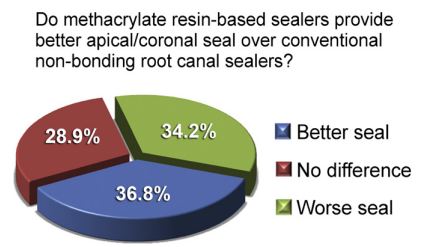
Till date four generations of methacrylate resin–based sealers (MBRS) have been introduced.
The first generation MBRS contained poly [2-hydroxyethyl methacrylate] as major ingredient was marketed as Hydron.
Second generation MBRS are hydrophilic and does not require etching to the adjunctive use of a dentin adhesive Eg; ENDOREZ.
The third generation sealers involve the use of a self-etching primer and dual-cured resin composite Sealer Eg; RESILON/EPIPHANY.
Lastly the fourth generation sealers, where in the etchant, primer and sealer were incorporated into an all-in-one self-etching, self-adhesive sealer Eg; METASEAL.
Teeth with significant loss of structure require posts in the interest of retaining the core. Since the currently favored fibre posts are passively retained into the root canal, an adhesive cement is important for a good seal. These cements may be categorized as Total-Etch Resin Cements, Self-Etch Resin Cements and Self-Adhesive Resin Cements.
Thus both MBRS and resin cements play a central role to achieve a monoblock, in that high bond strengths are imperative between the dentin and sealer/ cement, as well as between the sealer/cement and obturating material / post system.
Based upon the interfaces monoblocks are classified in to
Primary monoblock
Secondary monoblock
Tertiary monoblock.
1. Primary Monoblock
 |
| Primary Monoblock |
A primary monoblock has only one interface that extends circumferentially between the material and the root canal wall.
 |
| Primary Monoblock |
Hydron
MTA
Polyethylene fibre post-core systems
Biogutta
iRoot SP (EndoSequence BC Sealer)
Hydrone
 |
| Hydron |
Introduction
In the late 1970s, a Poly HEMA containing root filling material (Hydron; Hydron Technologies) was marketed for en mass filling of roots. The material garnered significant interest as a potential successor for sealer-dependent lateral and vertical gutta-percha (GP) obturation.
Advantage
Its purported qualities included ease of use, nonirritating nature, adaptability to walls, and ability to calcify in the event of extrusion.
Disadvantage
However this material became obsolete in the 1980s in view of discrepancies between the manufacturer’s claims and laboratory/clinical findings.
Hydron-filled root canals exhibited extensive leakages and Residual moisture within root canals notably hampered polymerization to form soft hydrogels that were extremely permeable and leachable.
Modulus of elasticity of Hydron ranges from 180 to 250 MPa. On the contrary in order to reinforce roots, the modulus of elasticity of a root filling material would need to approximate that of dentin (i.e., 14,000 MPa).
 |
| Apical and Coronal sealing of resin based sealer |
MTA
 |
| MTA fillapex Sealer |
Introduction
MTA is a Calcium silicate based material that has been made available since 1998
Used as an apexification material represents a contemporary version of the primary monoblock in attempts to strengthen immature tooth roots
MTA is composed principally of Portland cement with the addition of bismuth trioxide to render it radiopaque
Advantage
It is prudent to point out that the so-called high push out bond strength (ca. 38–40 MPa).
Interaction of the released calcium and hydroxyl ions of MTA with a phosphate-containing synthetic body fluid results in the formation of apatite-like interfacial deposits. The formation of these nonbonding, gap-filling apatite deposits probably also accounts for the seal of MTA in orthograde obturation and perforation repair.
The compressive elastic modulus of Portland cement increases after 14 days to 15 GPa (i.e., 15,000 MPa). Unlike Hydron, MTA should theoretically be able to strengthen roots.
Ability to stimulate cementogenesis in apexification and root end fillings
Disadvantage
Being an entirely inorganic material, Portland cement undergoes chemical shrinkage after hydration. Thus, a certain amount of volumetric shrinkage should also occur during the setting of MTA.
MTA is not bonded to dentin. The inability of MTA to strengthen roots is probably a combination of its lack of bonding to dentin and its low strength in tension, although it has high stiffness in compression
Polyethylene fibre post-core systems
 |
| Polyethylene glass fiber post |
A fiber composite laminate endodontic post and core system based on a woven polyester bondable ribbon had been introduced. This reinforcement material is composed of plasma treated ultra-high molecular weight polyethylene fibers woven into three dimensional structure, leno wave or triaxial braid.
Polyethylene fibre post-core system such as Ribbond (Ribbond Inc., Seattle, WA, USA) can create a primary monoblock in a root canal.
Impregnation of polyethylene fibre with a dual curable adhesive system (Belli & Eskitascioglu 2008).
Impregnated fibre is then condensed into the root canal in combination with a dual curable resin cement
Moreover fibres adapt well to root canal hence significant canal enlargement is not necessary. bonding agent to build-up endodontic posts and cores.
MOE similar to dentin.
A study by Singh et al reported that cyclic loading reduced the retention of all posts but was lesser for the polyethylene posts compared to glass fibre posts.
Similarly data on leakage studies indicate resin-supported polyethylene fiber dowels and glass fiber dowels tested exhibited less microleakage compared to zirconia dowel systems.
it provides good fracture resistance with increased incidence of repairable fractures in structurally compromised canals
However, a study by Jindal et al reported that endodontically treated teeth restored with
glass fiber posts showed increased fracture strength and favorable mode of fracture as compared to poloethylene fibre posts.
Biogutta
 |
| Biogutta |
A recent addition to the category of primary monoblock in denstistry is the Biogutta. This product contains bioactive glass of the 45S5 [The 45S5 name signifies glass with 45 wt. % of SiO2 and 5:1 molar ratio of Calcium to Phosphorus] type incorporated into polyisoprene, the matrix polymer of gutta-percha.
Bio GP Points composed of bioceramic materials creates monoblock obturation in canal wall with bioceramic-based sealer.
 |
| Biogutta primary monoblock |
Manufacturers claim the material is self-adhesive with immediate sealing of the canal system.
This has been attributed to the formation of Calcium Phosphate crystals on the material’s surface in a wet environment.
Preliminary studies report good push out bond strength to the canal dentin when compared with conventional gutta percha.
iRoot SP
 |
| iRoot SP |
Injectable Root Canal Sealer (Innovative BioCeramix Inc., Vancouver, BC, Canada), is an example of a calcium phosphate silicate-based cement.
These are convenient, premixed, ready-to-use, injectable white cement paste developed for permanent root canal filling and sealing applications.
2. Secondary Monoblock
 |
| Secondary monoblock |
These materials consists of two circumferential interfaces, one between cement/Sealer and dentin and other between the cement/Sealer and core material.
 |
| Secondary monoblock |
Examples
Resilon based systems
Fibre re-inforced posts.
iRoot SP with Gutta-Percha
By definition, conventional root canal obturations may be regarded as secondary monoblock systems on account of the two interfaces (one between sealer and dentin, second between sealer and conventional guttapercha condensed into a homogenous mass).
However the lack of sealer bond to dentin or guttapercha and the trivial values of modulus of elasticity (80 MPa) that are 175–230 times lower than dentin are contrary to the fundamental concepts of the ‘monobloc effect’.
Resilon
Resilon (2004) is a thermoplastic, synthetic, polymer-based obturation material
it is the first true bondable root canal filling material.
it is composed of dimethacrylate resin, bioactive glass as a filler, bismuth oxychloride, radiopaque barium sulfate, and polycaprolactone
 |
| Resilon Epipheny |
The system consists of three parts:
1. Resilon – a thermoplastic synthetic polymer-based (polyester) root canal filling material, as the major component;
2. Epiphany sealer – a dual-cure methacrylate resin-based composite
3. Self-etching primer - which prepares the canal wall to get in contact with Resilon and the sealer.
Resilon core closely adapting to the EpiphanyTM sealer and in turn the EpiphanyTM sealer adhering to the dentin walls via “resin tags”(mono-block)
The possibility that Resilon filled canals would be more able to withstand bacterial penetration as a result of this “Resin Monoblock System (RMS)”
Various techniques can be employed to place this material in the canal-
• Single-cone Method
• Cold Lateral Condensation
• Thermoplastic Techniques
Resilon is the only bondable root filling material that may be used for either lateral or warm vertical compaction techniques.
In one study, Epiphany root canal filling system exhibited the least coronal leakage when compared to gutta-percha and AH 26 sealer as well as gutta-percha and AH plus sealer.
However the study by Bodrumlu & Tunga showed no differences in apical sealing ability between Resilon/Epiphany and gutta-percha/AH Plus groups.
Disadvantage
Polymerization shrinkage occurs that can create gaps between the dentin and sealer
Impossible to achieve complete polymerization of the material especially in long narrow spaces.
Unpolymerized monomers can leach out of the material into a wet environment and promote bacterial growth
Resilon is biodegradable by cholesterol esterase and pseudocholinesterase
Glass Fiber Post
The modulus of elasticity of Resilon was found to be 86.6 ± 43.2 MPa under dry conditions and 129.2 ± 54.7 MPa after one month of water sorption
Thus, similar to gutta-percha, Resilon is not stiff enough to achieve a mechanically homogeneous unit with root dentin.
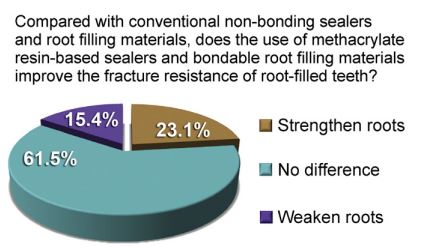 |
| Resin Based Sealer and Fracture Resistance |
Glass Fiber Post
Prefabricated post systems bonded to root canal dentine via resin cements represent a secondary monoblock.
First implied existence of a mechanically homogeneous monoblock was reported in 1996 with the bonding of epoxy resin– based, carbon fiber–reinforced posts to root dentin.
First implied existence of a mechanically homogeneous monoblock was reported in 1996 with the bonding of epoxy resin– based, carbon fiber–reinforced posts to root dentin.
Carbon fibers are made to bond to epoxy resins by means of an oxidative process.
Authors claimed that carbon fiber posts, having an MOE similar to that of dentin, could achieve a tooth–post– core monoblock.
 |
| Glass Fiber Post |
In the fiber posts the epoxy resin matrix are replaced with highly cross-linked , methacrylate resin matrices that have the potential to bond to methacrylate-based resin cements.
 |
| Panavia F |
Disadvantage
it was found that the carbon fibres are no longer surface active once the post is exposed by roughening during handling /with bur with resultant deterioration of bond to the epoxy resin matrix.
Secondly while carbon fibers have a tensile modulus (500 –1000 GPa) that is 2.5–5 times as strong as that of steel, its stiffness of carbon fiber is lowered by presence of epoxy resin.
Lastly epoxy resin is not bondable to methacrylate based resin sealer under physiologic temperatures.
3. Tertiary Monoblock
Tertiary monoblocks are those in which a third circumferential interface is introduced between the bonding substrate and the abutment material.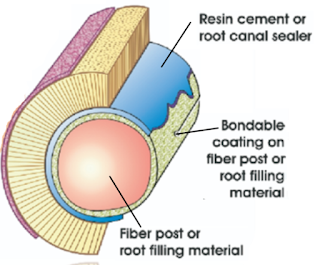 |
| Tertiary monoblock |
Examples-
EndoRez
Fiber Post + External Silane
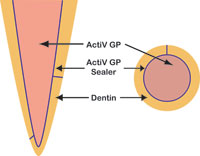
ActiV GP
EndoRez
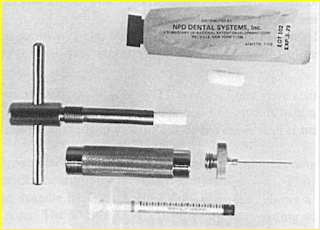
EndoREZ (Ultradent Products, South Jordan, UT) employs conventional gutta-percha cones coated with a proprietary resin coating to be used with a dual cured radiopaque methacrylate sealer.
 |
| Endorez |
In this system the mixed sealer is first syringed into canal by passive injection, using Navi tips followed by passive insertion of resin coated GP cones.
Disadvantage
Polymerization shrinkage of sealer, weak bond of sealer to the prepolymerized coating on guttapercha and lack of free radicals for adequate bonding.
Inconsistencies in the resin coating have been observed in the form of uneven circumferential thickness or partial detachment.
Fiber Post + External Silane
Fiber posts that contain an external silicate coating.
Coating made of silane and silicate is applied to the post
Fiber posts that contain an external silicate coating.
 |
| Tertiary Fiber Post |
Coating made of silane and silicate is applied to the post
Stiffer gutta-percha cone is achieved that transforms it into a gutta-percha core/cone, enabling the later to function as both the tapered filling cone and as its own carrier core.
However, being a single cone technique, coronal leakage of the ActiV GP system to fluid filtration was worse than that achieved with gutta-percha/AH Plus.
Conclusion
Although the concept of monoblock in endodontics is creating a mechanically homogenous units with root dentin is excellent in theory, accomplishing these “ideal monoblocks” in the root canal space is easier said than done.